In minimally invasive and image-guided procedures, visibility defines precision. Physicians rely on fluoroscopy, X-ray, CT, and hybrid imaging systems to guide catheters, stents, guidewires, delivery systems, and implantable components. If the device cannot be seen clearly on the monitor, the entire procedure becomes harder, slower, and riskier.
Radiopacity is what provides that clarity. As next-generation medical devices become smaller, more flexible, and more integrated with robotic systems, radiopacity is turning into a core design requirement. For many applications, the way radiopaque features are integrated during extrusion is just as important as the choice of material.
What Radiopacity Means in Medical Devices
Radiopacity refers to the ability of a material to block X-rays so it appears bright or white on imaging. This brightness makes it possible for clinicians to track a device during placement.
By contrast, radiolucent materials allow X-rays to pass through and appear dark on imaging. Radiolucent components are used intentionally when a device should not obstruct the view of anatomy or adjacent tools. For example, balloon materials or transparent housings are radiolucent by design.
Understanding radiolucency vs radiopacity is fundamental in device engineering. Many modern devices strategically combine both characteristics so only the critical areas are visible.
For background, the FDA provides general guidance on clinical imaging systems.
Radiolucency vs Radiopacity in Medical Devices
Radiopacity and radiolucency describe how materials interact with X-rays, and both are used intentionally in device design.
Radiopacity
- Blocks or absorbs X-rays
- Appears bright or white on imaging
- Used for markers, tips, reinforcement, and components that must be tracked in real time
Radiolucency
- Allows X-rays to pass through
- Appears dark or nearly invisible
- Used for balloons, outer jackets, housings, and areas where device visibility should not obscure anatomy
Engineers often combine both characteristics within the same device. Radiopaque features guide placement, while radiolucent regions preserve the view of surrounding anatomy and tools.
Why Radiopacity Matters for Next-Generation Procedures
As device geometries shrink and procedures rely more heavily on imaging, radiopacity has become a foundational performance requirement rather than an optional feature. Its impact shows up across several critical areas.
Precision in navigation
Vascular and neurovascular procedures often require millimeter-level accuracy. Radiopaque markers or shafts help clinicians determine tip position, rotation, and depth.
Safety
Better visibility reduces the risk of misplacement and shortens procedure time, which helps reduce overall radiation exposure.
Compatibility with robotic systems
Robotic angiography and image-assisted systems rely on fast interpretation of device movement. Radiopaque markers simplify that process.
Visibility in miniaturized devices
Microcatheters and thin-wall components can be difficult to track. Radiopaque materials restore essential contrast without changing dimensions.
How Radiopacity Is Created: Fillers and Material Choices
Radiopacity is achieved by compounding polymers with dense fillers known as radiopacifiers. These materials attenuate X-rays by absorbing or scattering photons, creating bright contrast on the imaging screen.
Common radiopaque fillers include:
Barium sulfate, the industry standard radiopacifier.
- Used in general catheter tubing
- Effective at 20 to 40 percent loading
- White in color and compatible with many medical-grade polymers
Bismuth compounds, preferred when higher contrast is needed.
- Twice as dense as barium
- Available as bismuth trioxide, subcarbonate, or oxychloride
- Useful in thin-wall or high-contrast applications
Tungsten, an ultra-dense metal powder for maximum visibility.
- Excellent for microcatheters
- Strong attenuation at relatively low volume
- Requires precise compounding and extrusion control
In many cases, blending fillers produces the best overall performance across a range of fluoroscopy and X-ray energy levels.
How Extrusion Enables Radiopaque Designs
This is where Medical Extrusion Technologies provides real value. Radiopaque features are often integrated directly during the extrusion process. The way materials are distributed, layered, or co-extruded determines how well the final device will appear under imaging.
Key extrusion-driven approaches include:
Compounded radiopaque tubing
Fillers are blended into the polymer before extrusion to create a consistently visible shaft, as seen in profile extrusion.
Radiopaque stripes
A thin radiopaque stripe is co-extruded along a radiolucent shaft, as seen in multi-lumen tubing. This preserves flexibility while offering a clear positional indicator.
Selective radiopacity in multi-lumen tubing
Only the lumen requiring visibility receives radiopaque material. This is common for guidewire channels or contrast-delivery lumens.
Radiopaque markers
Co-extruded markers or localized radiopaque sections allow designers to highlight tips, junctions, or areas of interest without adding extra components.
These methods ensure radiopacity is designed into the tubing without compromising profile size or mechanical performance.
Balancing Visibility With Performance
Radiopacity must be engineered carefully to avoid degrading mechanical properties. Factors that influence performance include:
- Filler loading levels
- Particle size and dispersion
- Wall thickness and concentricity
- Extrusion temperature and mixing behavior
- Beam energy of the imaging system
High-density fillers can cause loss of tensile strength or unwanted stiffness if overloaded. This is why OEMs often work closely with extrusion partners early in the design process.
Materials used in radiopaque tubing must also meet biocompatibility criteria outlined in ISO 10993.
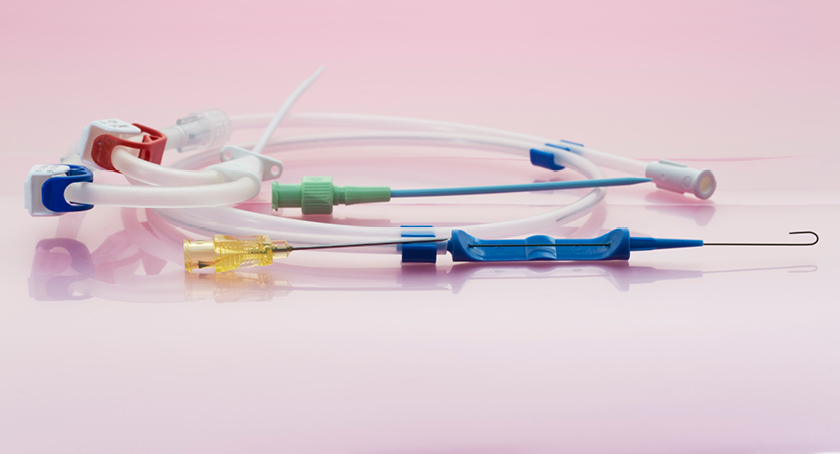
Where Radiopacity Is Used in Modern Devices
Radiopaque tubing plays a critical role in:
- Cardiovascular catheters
- Neurovascular microcatheters
- Structural heart delivery systems
- Biliary and GI stent systems
- Electrophysiology catheters
- Sheaths and introducers
- Robotic systems with imaging overlays
As device geometries become more advanced, radiopaque features are becoming integrated into more components, not fewer.
The Future of Radiopaque Materials
Emerging advancements include:
- Nano-filled radiopaque polymers for improved dispersion
- Hybrid blends of barium and bismuth optimized for modern fluoroscopy energy levels
- Radiopaque bioresorbable polymers
- Micro-extrusion techniques for ultra-small vascular devices
MET supports OEMs working across these new material landscapes by refining extrusion parameters, optimizing filler integration, and helping validate material choices through tensile and dimensional testing.
Ready to Develop Radiopaque Tubing
Radiopacity is a central element of modern device engineering. Whether you are designing a new catheter shaft, a microcatheter tip, or a delivery system for structural heart therapies, visibility on imaging determines precision and safety. To explore radiopaque tubing, radiopaque stripes, multi-lumen configurations, or custom extruded solutions for advanced devices, connect with the team at MET.






Comments are closed